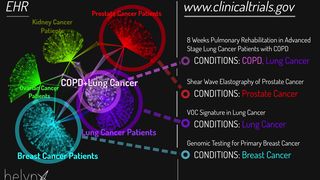
In a survey of over 400 cancer patients, the most common reason patients gave for not participating in trials was lack of awareness of trials appropriate for them (1). Likewise, 43% of oncologists reported that finding trials closeby was an obstacle to referring patients for clinical trials, while 33% reported that learning about inclusion/exclusion criteria of clinical trials was an obstacle. A systematic review of studies on clinical trial accrual also reported that lack of awareness of trials is one of the most common obstacles to accrual (2). To that end, the National Cancer Institute and American Society of Clinical Oncology have recommended the use of information technology to identify potentially eligible patients (3) in order to target and communicate with them more efficiently and effectively.
Our system identifies patients eligible for trials, but does not actually enroll patients in the trials. Physicians must act upon the information, by engaging patients and referring them to eligible trials. Based on focus group data, City of Hope community oncologists have a positive attitude towards clinical trials and feel that an electronic tool to identify eligible patients would be helpful. One strength of our software is the ability to learn from experience to fine tune the functionality. We will periodically analyze the data and meet with the practitioners to improve the experience.
50%. A similar computer-aided eligibility screening system was able to increase clinical trial enrollment at a single cancer center, and we believe that our system will be more robust due to advances in the EHR and computing tools. The satellite clinics’ trial enrollment figures for the last several years provide solid baseline against which to compare enrollment. Using chart review, we will assess the rate of clinical trial participation at each clinic both before and after the system is implemented. Additionally, we can include a short questionnaire in the message to physicians.
If our system works as we expect, we believe it will build trust within the physician community. If the tool improves provider and patient satisfaction, it could easily be incorporated permanently into the EHR. This kind of integration would make the system even easier to use by physicians during patient encounters.
In this case, the use of patient data is fully HIPAA (Health Insurance Portability and Accountability Act) compliant. Helynx uses data load, storage and dissemination processes that are HIPAA compliant, and has multiple layers of safeguards against security breach. Whenever possible, such as during the data analysis and system build-out phase, patient-identifying information is removed or anonymized, so that personal patient health data are never compromised. The final system will run on a secure, cloud-based server, subject to independent audit.
A computer-aided eligibility tool has been previously used to increase enrollment in breast cancer trials. However, the incompleteness of the EHR and computing limitations prohibited wider adoption. EHR comprehensiveness has evolved dramatically over the last half-decade, as have advances in machine learning, and software packages such as Helynx itself, each of which have contributed to improvement in clinical and research outcomes. This proposal may represent the first fusion of these techniques to solve the problem of patient identification for clinical trial enrollment.